There are many different thoughts as to why chronic pain occurs. The most obvious reason for chronic pain is continued tissue irritation as a result of a failure to modify a pain causing behavior. This basically occurs when a person continues to participate in activities that overload and damage already injured tissue. An example of this would be returning to a job requiring repetitive movements such as lifting when this is the activity that resulted in injury in the first place. This is especially true if this injury never had a chance to fully heal in the first place. In these cases of chronic pain, clearly rest and activity modification is required to resolve chronic pain.
What about the cases where the aggravating activity has been modified or discontinued, the tissue is allowed to properly heal, and a patient still has pain? These are the cases where chronic pain becomes very difficult to treat and causative factors are difficult to identify. We’ll provide a quick overview of why this occurs. One of the main reasons researchers believe chronic pain is such a puzzle are changes that occur in the central nervous system (brain and spinal cord) as a result of chronic pain.
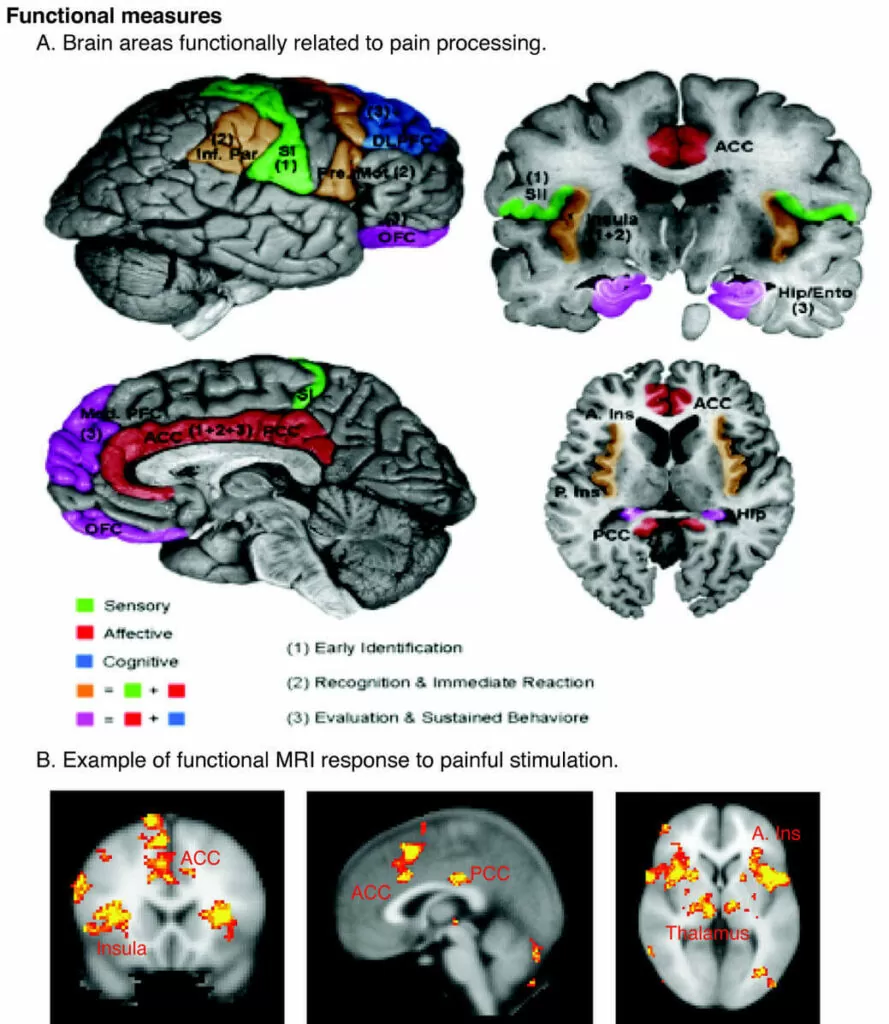
One of the main changes that can occur in the central nervous system is a condition called central sensitization (CS). This condition is though to arise when neurons in the spinal cord become over-excitable due to repeated painful stimuli.1 This means the neurons in the spinal cord are more likely to send a pain signal to the brain, which increases the brain’s responsiveness to pain. To clarify painful stimuli that would not normally be transmitted to the brain are now sent and are registered as more painful than they were previously. This also results in a longer lasting pain experience after the stimulus is removed.1,2
To further complicate the problem, CS can increase the ability of non-injured tissue to produce pain.1 What’s worse, as the phenomenon of CS progresses, non-painful stimuli may be interpreted as painful stimuli.1 Research has demonstrated that after CS is induced, the brain can interpret light stroking of the skin as pain even in areas distant to the site of injury.1 The same research demonstrated sensitivity to light touch in these areas did not respond to injection of a local anesthetic. This indicates processing of this pain experience occurred in the brain and spinal cord versus the nerves in that area.
When CS is allowed to progress without proper intervention some patients become unable to tolerate any type of light touch. Some patients have even reported marital problems, as they cannot tolerate their spouses touching them anywhere on their body no matter how light the touch. Others have reported an inability to wear certain types of clothing due to skin sensitivity. When chronic pain gets to this level proper intervention is necessary to restore quality of life. So what can be done to treat this pain and reverse sensitization that has occurred in the central nervous system?
I first began writing this blog post in response to the huge opioid epidemic that has struck the United States. Addiction to opioids and deaths due to overdoes of opioids are becoming so common that the Virginia Department of Health declared the opioid epidemic a public health emergency on November 21, 2016. Opioids are common medications that are prescribed for the management of chronic pain. These medications however are not good long-term management solutions as they can be habit forming and they do not function to address the condition that caused pain in the first place, they merely mask the symptoms.
Now, that you have an understanding of the basic physiology, we will discuss what can be done to manage chronic pain. The first important step to addressing pain is to have a basic understanding of pain. I hope you have gained some insight from these two blog posts. Another great resource is the video located here: https://www.youtube.com/watch?v=5KrUL8tOaQs, which explains pain in less than 5 minutes.
The next step is identifying and treating any injury or dysfunction throughout the body that may be resulting in nociceptive (painful) input to the brain. As you can understand from reading these blog posts and watching the video, this is easier said than done. With the presence of phenomena such as CS and referred pain it may be hard to determine problematic areas, as pain may be widespread or located in areas distant to the problem site. For this reason, a thorough clinical examination consisting of movement assessment and palpation must be performed to accurately identify problematic areas in the body.
As physical therapists we have a thorough understanding of normal movement and tissue function throughout the body. This allows us to accurately identify problematic areas in order to design a treatment program to treat pan and dysfunction. We also have a wide variety of effective treatment interventions including dry needling, Fascial Manipulation®, and Postural Restoration Institute® techniques that allow us to address the underlying problem, not merely mask the symptoms. For more information on what we can do to help with your pain please contact our office to schedule an appointment. If you are unsure if physical therapy is appropriate for your condition, we offer free 10 minute phone consultations and screenings for your convenience.
Sources
- Woolf, C. J. (2011). Central sensitization: implications for the diagnosis and treatment of pain. Pain, 152(3), S2-S15.
- Mense, S. (2008). Muscle pain: mechanisms and clinical significance. Dtsch Arztebl Int, 105(12), 214-9.
Tags: Fascial Manipulation, Diagnosis, Patient Care, Postural Restoration